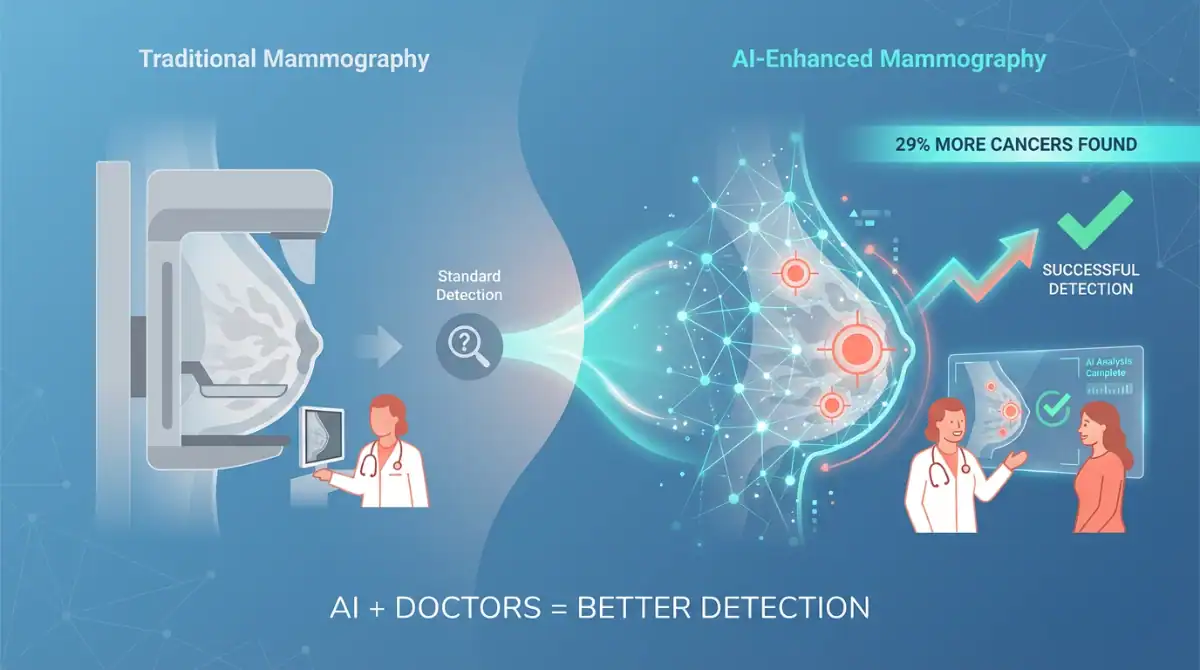
AI Helps Doctors Detect 29% More Breast Cancers
Swedish researchers find AI-supported mammography catches more cancers earlier and reduces aggressive cases but emphasize the technology must support—not replace—human doctors.
Key Points
- AI-supported screening detected 29% more breast cancers compared to standard double-reading by radiologists
- Interval cancer rate (cancers found between screenings) reduced by 12% with AI assistance
- AI system cut radiologists’ screen-reading workload by 44% without compromising accuracy
- Study involved over 105,000 women in Sweden’s national screening program (2021-2022)
- Researchers emphasize AI supports doctors—it doesn’t replace them
Background
Breast cancer remains one of the world’s deadliest diseases, causing an estimated 670,000 deaths globally in 2022 according to the World Health Organization. In Europe, mammograms are typically read by two radiologists independently—a process called double reading—to ensure accuracy. However, radiologist shortages worldwide have put strain on screening programs, and some cancers still slip through, appearing as “interval cancers” diagnosed between regular screenings.
The Mammography Screening with Artificial Intelligence (MASAI) trial was designed to test whether AI could help solve these challenges. This groundbreaking study, led by Dr. Kristina Lång from Sweden’s Lund University, represents the first completed randomized controlled trial—the gold standard in medical research—evaluating AI in breast cancer screening.
What Happened
Between April 2021 and December 2022, researchers randomly assigned over 105,900 women attending routine mammography screenings in Sweden into two groups. One group received AI-supported screening, while the other underwent standard double-reading by radiologists.
Here’s how the AI system worked: The Transpara AI software (version 1.7.0 by ScreenPoint Medical) first analyzed each mammogram and assigned a risk score from 1 to 10. Low-risk cases (scores 1-9) were reviewed by one radiologist, while high-risk cases (score 10) required two radiologists—the standard approach. The AI also highlighted suspicious areas on the scans to help doctors identify potential problems.
The full results, published in The Lancet and The Lancet Digital Health in January 2026, revealed impressive outcomes (ℹ️ The Lancet Digital Health):
- 338 cancers detected in the AI group versus 262 in the standard group—a 29% increase
- 24% more early-stage invasive cancers caught in the AI group (270 versus 217)
- 12% reduction in interval cancers over the two-year follow-up period (1.55 per 1,000 women with AI versus 1.76 per 1,000 with standard screening)
- 44% reduction in radiologist workload without compromising detection accuracy
- No increase in false positives—both groups had similar recall rates (1.5% for AI vs. 1.4% for standard)
“We found that we could detect more cancers when we screened with the support of AI. But at the same time, it did not increase false positives, and we can reduce the screen reading workload for radiologists by almost half,” Dr. Lång explained (ℹ️ Lund University).
Why It Matters
This research carries significant implications for breast cancer screening worldwide. The 12% reduction in interval cancers is particularly important—these cancers appear between regular screenings and are often more aggressive and harder to treat than those caught during routine scans.
The AI system detected more early-stage invasive cancers and aggressive subtypes that benefit most from early treatment. According to the study published in The Lancet Digital Health, catching these cancers earlier could lead to “reduced suffering, higher survival rates, and lower economic costs.” (ℹ️ ThePrint)
The dramatic reduction in radiologist workload addresses another critical issue: the global shortage of breast radiologists. By automating the review of low-risk cases, AI frees up specialists to focus on complex cases and other patient care duties.
Importantly, the technology didn’t replace doctors—it supported them. “Our study does not support replacing healthcare professionals with AI,” emphasized Jessie Gommers, PhD student at Radboud University Medical Centre in the Netherlands and first author of the study. “The AI-supported mammography screening still requires at least one human radiologist, but with support from AI.”
What’s Next
The Swedish findings have already inspired larger initiatives. The UK government announced the EDITH (Early Detection using Information Technology in Health) trial in February 2025, planning to enroll 700,000 women across 30 National Health Service sites using five different AI platforms—with £11 million in funding.
However, Dr. Lång cautioned against rushing implementation: “Introducing AI in healthcare must be done cautiously. Further studies and cost-effectiveness analyses will help clarify the long-term benefits and risks, especially as many countries face shortages of trained radiologists.”
The researchers also noted some limitations. The study was conducted in one country using one AI system and didn’t collect data on participants’ race and ethnicity. Questions remain about how well these results would translate to different healthcare systems, populations, and equipment.
For countries like India, where radiologist shortages are even more severe, implementing such technology would require different approaches and infrastructure, including robust cancer registries to track outcomes (ℹ️ DevDiscourse).
Deep Details
The MASAI trial’s success lies in its careful design and large scale. The median age of participants was 54 years, and the study achieved a two-year follow-up through Sweden’s comprehensive Regional Cancer Registry—an infrastructure that allows researchers to track every cancer diagnosis and ensure no cases are missed.
The AI system used in the trial was trained on over 200,000 mammography examinations from more than ten countries, giving it broad exposure to different breast cancer presentations. This training helped the system identify subtle patterns that might indicate early-stage cancers.
Crucially, the AI didn’t just detect more cancers—it found the right kinds of cancers. The study showed 51% more pre-cancerous lesions (ductal carcinoma in situ) were detected with AI support, catching potential problems before they become invasive.
The technology also maintained safety standards. False positive rates—when women are called back unnecessarily—remained virtually unchanged, meaning the improved detection didn’t come at the cost of added anxiety or unnecessary procedures for women.
Looking ahead, researchers plan to assess the cost-effectiveness of AI-supported screening and investigate whether earlier detection through AI translates into improved survival rates and reduced mortality—the ultimate measure of any screening program’s success.
Source Attribution
Source: The Lancet, The Lancet Digital Health, Lund University — Published January 30, 2026
Original articles:
About the Author
Abir Benali is a friendly technology writer specializing in making AI and medical innovations accessible to everyday readers. With a passion for translating complex scientific research into clear, actionable information, Abir helps non-technical audiences understand how emerging technologies impact their lives and health.